More than 1.2 million people—and potentially millions more—died in 2019 as a direct result of antibiotic-resistant bacterial infections, according to a landmark study published in The Lancet by the Global Research on Antimicrobial Resistance (GRAM) Project.
The analysis of 204 countries and territories by GRAM partners at the Institute for Health Metrics and Evaluation (IHME) and the University of Oxford reveals that resistance is now a leading cause of death worldwide, above of HIV/AIDS or malaria. It shows that many hundreds of thousands of deaths now occur due to historically treatable illnesses, including pneumonia, foodborne ailments, and hospital-acquired infections.
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, and parasites change over time and no longer respond to medicines—making infections harder to treat and increasing the risk of severe illness and death. GRAM estimated total deaths and disability from drug resistance observed in 23 different bacteria, and found that people of all ages and income-levels died from common infections in the lower respiratory tract, bloodstream, and intra-abdominal region.
Confirming the global urgency of AMR for the first time with comprehensive evidence, the report highlights the need to scale up action, and outlines immediate steps for policymakers to help save lives and protect health systems. These include optimising the use of antibiotics; doing more to monitor, prevent, and control infections; boosting clean water and sanitation resources; and, funding new antibiotic drug development.
“This paper is a critical step that allows us to see the full scale of the challenge,” said Prof Chris Murray, a study co-author and IHME Director. “We need to leverage this data to course-correct action and drive innovation if we want to stay ahead in the race against antimicrobial resistance.”
GRAM’s leadership in Oxford, Prof Christiane Dolecek, Dr Catrin Moore, and Prof Benn Sartorius, also called on policymakers to use the results to drive action.
“Being able to measure AMR, and compare it with other major health threats, is essential to addressing its serious consequences,” they said. Profs Dolecek and Sartorius are based in the Centre for Tropical Medicine and Global Health, and Dr Moore is based in the Big Data Institute. “This work incorporates the best available data and provides reliable evidence describing the substantial mortality and morbidity caused by AMR globally.”
Previous works have provided estimates of AMR health impacts for several countries and regions, and for a small number of pathogen-drug combinations in a wider range of locations. However, until now no estimates have covered all locations and a broad range of pathogens and drug combinations.
Funded by the UK Department of Health and Social Care, the Wellcome Trust, and the Bill and Melinda Gates Foundation, GRAM found that two bacteria each caused close to 200,000 deaths in one year from AMR: Escherichia coli, a common stomach bug, and Klebsiella pneumoniae, which often infects the lower respiratory tract. The study also tracked AMR in 88 separate bacteria-and-antibiotic combinations, finding that MRSA, or methicillin-resistant Staphylococcus aureus, which infects the skin and is often acquired in hospitals, is the “bug-drug” combination that caused the most deaths: more than 100,000.
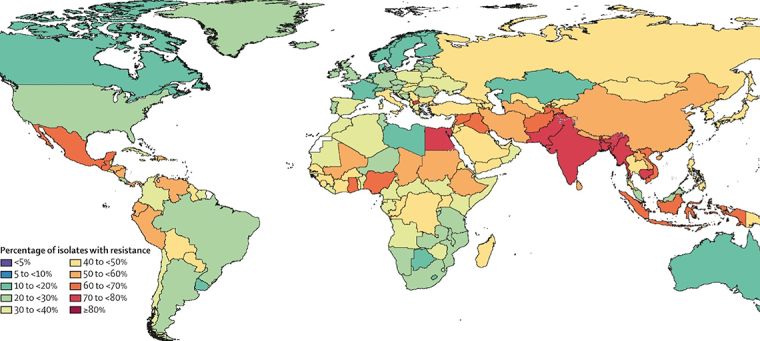
Applying methods and data not previously utilized in AMR studies, the report described AMR as a serious problem in both rich and poor countries, but most harmful in sub-Saharan Africa, which saw at least 255,000 deaths from resistance in one year, at a rate of 23.7 per 100,000.
Researchers estimated disease burden in two ways: deaths caused directly by AMR (i.e. deaths that would not have occurred had the infections been drug-susceptible and therefore more treatable), and deaths associated with AMR (i.e. where a drug-resistant infection was implicated in deaths, but resistance itself may or may not have been the direct cause). Deaths caused by and associated with AMR were calculated for 204 countries and territories and reported for 21 global regions and seven super-regions.
Although AMR has existed since the first modern antimicrobial treatments emerged in the 20th Century, health leaders have struggled to address a problem they believe has grown worse for multiple reasons, including improper use of medicines in human and animal populations, and insufficient measures to prevent and control infection.
GRAM produced the estimates by adapting and refining methodologies from IHME’s ongoing Global Burden of Disease (GBD) study. By providing better data on AMR-related mortality and morbidity policy makers can tailor interventions to regions most in need, focusing on specific bacteria and antibiotics relevant to those areas, authors said.
Growing concern
A previous study sponsored by the United Kingdom in 2016 led by economist Jim O’Neill estimated that AMR claimed at least 700,000 lives worldwide each year, and that without intervention the number could rise to 10 million annually by 2050. Although scientists have debated those figures—the O’Neill review did not publish its methodology—results provided an early snapshot of global AMR which included deaths from drug-resistant viruses, bacteria, parasites, and other pathogens.
The GRAM study, which covered bacterial AMR only, reported nearly twice as many deaths in one year than O’Neill. And because GRAM limited its focus to 23 clinically important bacteria, the results do not include AMR burden from all other pathogens – meaning the true scale of health loss is likely larger.
Seven drug-resistant bacteria caused more than 1 million deaths in 2019, according to GRAM: Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, Acinetobacter baumannii, Streptococcus pneumoniae, Pseudomonas aeruginosa, and Mycobacterium tuberculosis.
In sub-Saharan Africa, which had the highest levels of AMR burden, K. pneumoniae accounted for nearly 20 percent of deaths, with S. pneumoniae making up just over 15 percent. In high-income countries, including the United States, Germany, and Japan, S. aureus accounted for more than 25 percent of the 141,000 deaths from resistance.
After sub-Saharan Africa, GRAM found the highest proportion of AMR burden in South Asia, followed by Central and Eastern Europe, and Central Asia; Latin America and the Caribbean; North Africa and the Middle East; and, finally, high-income countries. Although AMR impacts people of all age groups, one in five deaths occurred in children under five.
The data challenge
To estimate global AMR burden GRAM relied on extensive new clinical evidence obtained from systematic reviews, and direct engagement with collaborators based in public health institutes, government ministries, academic institutions, and industry. Drawing from 471 million separate data points, GRAM also utilized data available from the GBD study.
Lack of data in many parts of the world, particularly low and middle income countries (LMICs), may limit the accuracy of estimates made with certain methodological assumptions.
Researchers said improving data collection worldwide—an exercise made easier now that gaps are more apparent—will lead to more accurate measures of AMR, and better health treatments.
AMR mortality and morbidity
In addition to reporting AMR mortality, GRAM also estimated morbidity, with disability-adjusted-life years (DALYs) measuring the total number of healthy years lost to illness or morbidity. Across all 23 pathogens, GRAM calculated 47.9 million DALYs due to AMR, with K. pneumoniae, E. coli, S. pneumoniae, and S. aureus causing the most disability overall.
The study also calculated AMR by infectious syndrome, showing the main disorders for which patients received treatment for a resistant infection. Lower respiratory infections caused the most deaths and DALYs overall – close to 400,000 deaths and 20 million DALYs – followed by bloodstream infections, which caused approximately 350,000 deaths and 15 million DALYs.
Although the GRAM study—titled “Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis”—measured AMR burden in one year only, the team hopes to add additional years in the future, with an aim to add AMR to the GBD study (1990 to the present) as early as 2023.
***
Members of GRAM will join other speakers at a webinar to discuss the AMR results, on Friday, 4 February from 17.00 to 18.30 GMT. Sponsored by the Wellcome Trust, UK Department of Health and Social Care and Bill and Melinda Gates Foundation, the event is open to the public. For more information or to register visit the Wellcome Trust.