Antimicrobial resistance (AMR) is linked to more than 1 million disease-related deaths in Africa, the Global Research on Antimicrobial Resistance (GRAM) Project has reported in a new paper in Lancet Global Health.
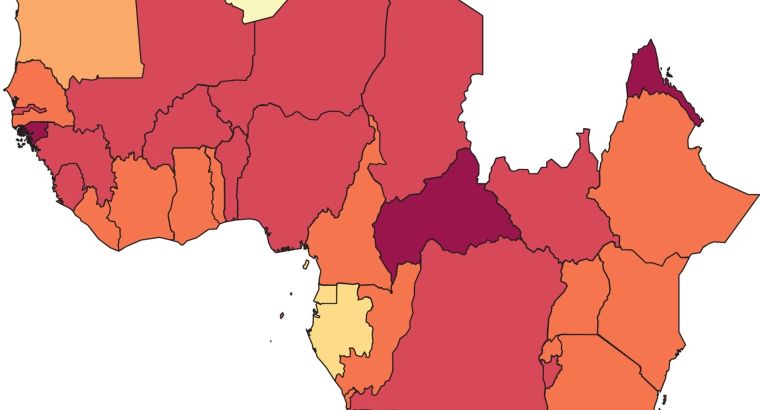
One of the most comprehensive regional- and country-level estimates of AMR burden to date, the study found that 1.05 million people across 47 countries in the WHO Africa Region died with a drug-resistant infection—more than 21 percent of the global total and one of the highest levels overall. GRAM, a partnership between the University of Oxford and the Institute for Health Metrics and Evaluation (IHME) in Seattle, reported the findings as part of its analysis of AMR in 2019.
Deaths associated with AMR are fatalities that occur when a patient dies with a drug-resistant infection. In such cases, resistance may or may not be the cause of death, for example, if individuals have other underlying conditions responsible for the outcome. But the figures nevertheless point to large-scale prevalence of AMR.
The paper also found that AMR directly caused 250,000 deaths in Africa. These so-called attributable deaths are those in which patients died precisely because their resistant infections were not treatable. In these cases, AMR is considered the cause of the death.
‘The alarming burden of AMR in Africa calls for more urgent and targeted interventions in the region’, said co-first author Dr Benn Sartorius, a GRAM senior investigator based in Brisbane, Australia. ‘This study we hope paves the way for such action’.
The findings underscore the rising global health threat from AMR. In 2022, a landmark GRAM study found that AMR directly caused at least 1.27 million attributable deaths, but that up to 4.95 million people died with a drug-resistant infection.
Based on attributable deaths, the team identified AMR as a leading cause of death worldwide, above HIV/AIDS or malaria. However, the larger toll of deaths associated with drug resistance would make AMR the third leading cause of death, behind only ischaemic heart disease and stroke.
GRAM is funded by the UK Department of Health and Social Care’s Fleming Fund, the Wellcome Trust, and the Bill and Melinda Gates Foundation.
More than 800,000 deaths associated with resistance in Africa occurred from seven leading bacterial pathogens. Four of these each caused 100,000 AMR-associated deaths: Streptococcus pneumoniae, Klebsiella pneumoniae, Escherichia coli, and Staphylococcus aureus.
The study estimated deaths and disability adjusted life years (DALYs) attributable to and associated with AMR for 23 bacterial pathogens and 88 pathogen-drug combinations.
Unlike other regions, researchers found no correlation between high burden rates in Africa and lack of AMR national action plans. They also found no link between decreasing resistance and increasing states of NAP development.
Lack of data in many parts of the world, particularly low and middle income countries (LMICs), may limit the accuracy of estimates made with certain methodological assumptions. Researchers have said improving data collection worldwide will lead to more accurate measures of AMR, and better health treatments.
In the future, GRAM hopes to incorporate AMR into IHME’s regular Global Burden of Disease study, so that drug resistance is measurable and comparable to other types of health loss over time.