Global burden of bacterial AMR
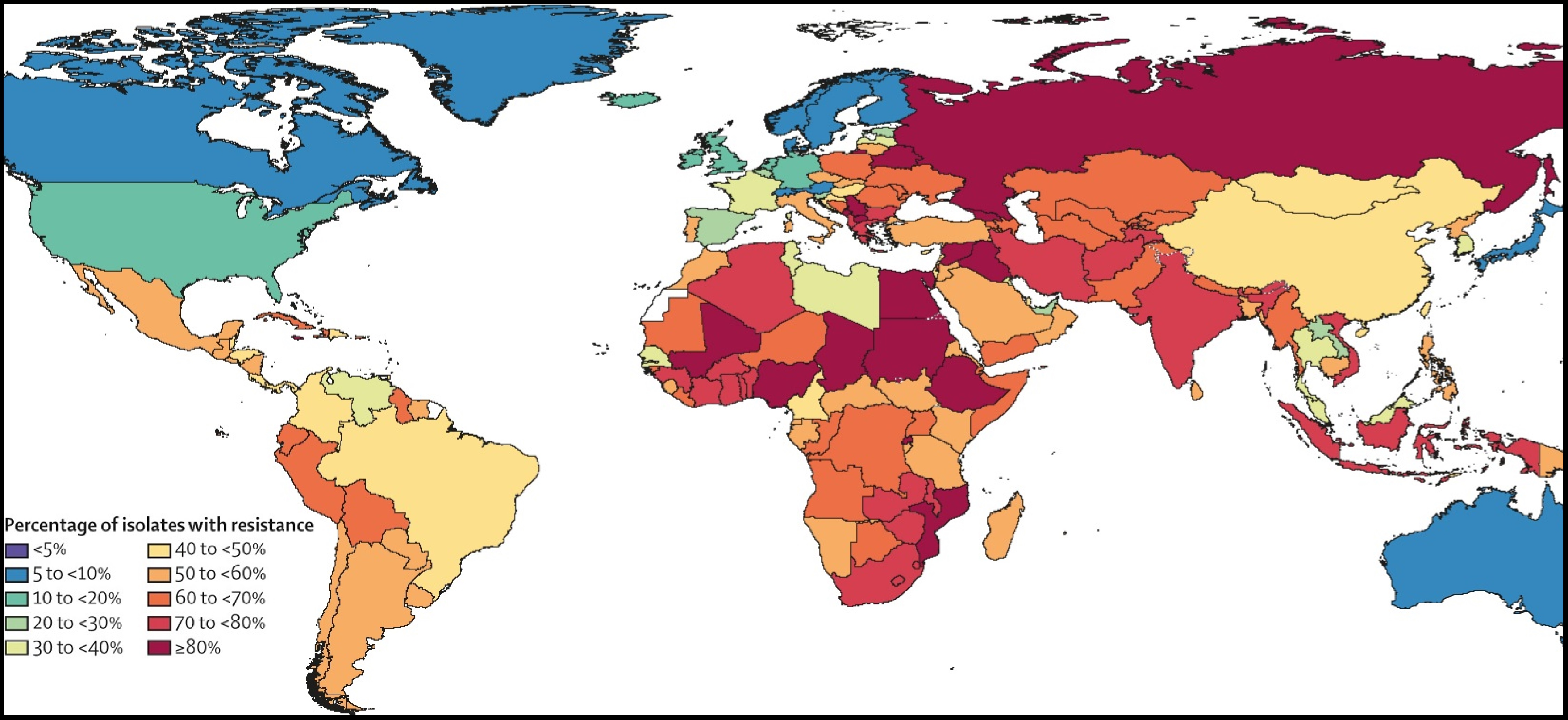 Third-generation cephalosporin-resistant Klebsiella pneumoniae by country and territory, 2019GRAM provides a critical measure of global antimicrobial resistance (AMR) for researchers, health practitioners, and policymakers: the global burden of bacterial AMR. Faced with data sparsity, incomplete surveillance, and other challenges, GRAM applies methodologies developed in the ongoing Global Burden of Disease (GBD) study to estimate the impact of drug-resistant bacterial infections on global deaths and disability. Our research seeks to inform location-specific policy decisions about infection prevention and control, access to antibiotics, development of new drug treatments and vaccines, and other public health matters.
Third-generation cephalosporin-resistant Klebsiella pneumoniae by country and territory, 2019GRAM provides a critical measure of global antimicrobial resistance (AMR) for researchers, health practitioners, and policymakers: the global burden of bacterial AMR. Faced with data sparsity, incomplete surveillance, and other challenges, GRAM applies methodologies developed in the ongoing Global Burden of Disease (GBD) study to estimate the impact of drug-resistant bacterial infections on global deaths and disability. Our research seeks to inform location-specific policy decisions about infection prevention and control, access to antibiotics, development of new drug treatments and vaccines, and other public health matters.
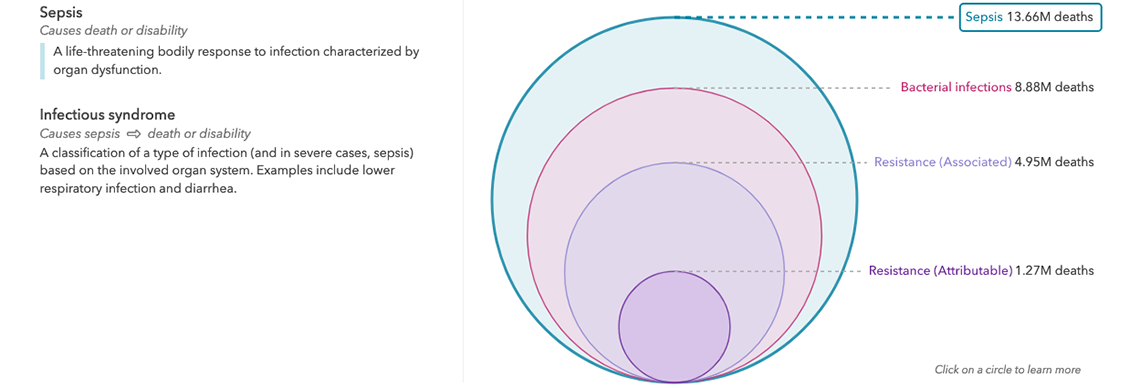
Our research provides the first comprehensive estimate of AMR burden in 204 countries and territories. Utilizing data obtained from systematic literature reviews, hospital systems, surveillance networks and other sources, we apply statistical modelling to produce estimates of bacterial AMR burden worldwide. GRAM provides two separate counterfactual estimates of death and disability from AMR: burden attributable to AMR (based on an alternative scenario in which all drug-resistant infections were replaced by drug-susceptible infections), and burden associated with AMR (based on an alternative scenario in which all drug-resistant infections were replaced by no infection). While burden attributable to AMR links resistance directly to health outcomes, burden associated with AMR assumes that resistance may or may not have played a role in death or disability.
GRAM project findings for 2019 show that an estimated 4.95 million people died with a drug-resistant bacterial infection, and that more than 1.27 million of those deaths are directly attributable to AMR. The results confirm that bacterial AMR is a leading cause of death and disability worldwide, with a burden greater than either HIV/AIDS or malaria. Although AMR affects populations in both rich and poor countries, GRAM identified the highest burden levels in low-resource settings. Sub-Saharan Africa experienced the highest rate of AMR burden, with 23.7 deaths per 100,000 people, while Australasia had the lowest, at 6.5 deaths per 100,000. Tracking resistance in 88 separate pathogen-and-antibiotic combinations, researchers found that seven leading bacteria (in order) caused more than one million attributable deaths in 2019: Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, Acinetobacter baumannii, Streptococcus pneumoniae, Mycobacterium tuberculosis, and Pseudomonas aeruginosa. The first two, Escherichia coli and Klebsiella pneumoniae, each caused close to 200,000 deaths. MRSA, or methicillin-resistant Staphylococcus aureus, is the pathogen-antibiotic combination which caused the most deaths: more than 100,000. In addition to mortality, our work also measures the burden of morbidity from bacterial AMR, in the form of disability-adjusted-life years, shown by region, bacteria, and antibiotic class.
Explore the data