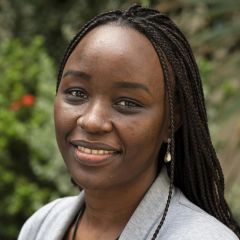
Naomi Waithira: Data, science and health
MORU Data Management focuses on tropical infectious diseases, gathering data from diverse sources like patient interviews, medical records and laboratory results. This data, stripped of identifying information, is organized for analysis. Past clinical data aids new insights, augmented by mathematical modelling and AI. MORU aims to improve healthcare by leveraging technology for accurate, impactful solutions.
My name is Naomi Waithira. I head the data management group at MORU Tropical Health Network. In my group, we work with medical experts and researchers to conduct clinical studies, with our focus being on infectious diseases that affect the populations in the tropics. This includes diseases caused by bacteria, viruses, or other organisms.
In the course of the clinical studies, we collect information from various sources to help us determine whether certain drugs are safer or more effective at treating diseases, and also, to identify drugs and vaccines that can be used to protect individuals from contracting specific diseases when they come into contact with. This data comes from a variety of sources. One example is through talking directly with a patient and asking them how they feel, and how the disease is affecting their daily life. A second source of data is through looking back at medical records to understand the history of the patient. Another data source is looking at laboratory results and imaging results. So, this data comes to us in the form of words, numbers and images (including X-rays or ultrasound recordings).
In the first step, we remove any parameters that could potentially identify the patient because we want to protect their privacy. We then organise this data in a way that can be understood by both humans and machines and used for analysis to draw conclusions of the research work, for instance, in determining whether drug A is more effective than drug B in treating malaria among pregnant women. In addition to that, we store this data securely, and only grant access to individuals who are authorised to do analysis based on the laws of the countries we are working in.
Clinical studies can be quite expensive, and they can also be time-consuming. Very often the data that's collected in a clinical study is used primarily for analysis of the research questions for that study. Once that's finished, the data is put away securely and safely. Now, is there a chance that we could use data that has been collected in past clinical studies to gain new insights on how diseases manifest, and also, to get ideas about what measures we could take in control of these diseases?
There are a lot of technological advancements that can help us to do that, including mathematical modelling and even more recently, we've seen a lot of progress in artificial intelligence. By using AI tools, we're able to equip medical professionals with information that could help them to diagnose and treat diseases more effectively. One application in mathematical modelling is when climate data, population data, and medical data are all combined to predict when seasonal diseases such as influenza would come back. Where would the outbreak likely be? Which populations are they likely to affect the most? With this information, government agencies can put in place measures to control the outbreaks, or even prepare for the outbreaks through public education, for instance.
By looking at this potential for use of informatics and AI in the field of medicine, we have an opportunity to transform the way medical care is delivered and in our fight against diseases. And in fact, using AI tools, patients themselves can interact with software from the comfort of their homes to get information about their condition. That would have come from a doctor, but they would have had to wait much longer would probably have had to travel a long distance, and maybe would cost them even more.
But one important thing to note about using AI, is that these tools need to be accurate and they need to be as knowledgeable, perhaps even more knowledgeable than a human doctor. How do we achieve that? For these tools to be accurate and to function the way they should, they need to be trained using high-quality data that is well-organised and well-linked. We are setting up pipelines that facilitate that, through collecting the data and then organizing it in a way that can be easily understood by both machines and humans. In addition to that, we're looking back at old datasets that were collected a long time ago. MORU has been in existence for about 50 years, so we're looking at fairly old datasets, and curating them to look like the datasets that we're currently generating. So overall, it is our hope that we're able to provide data that's of high quality, and that can be used for modelling and for artificial intelligence and various other types of analysis to generate key insights for the health of the community.
MORU conducts research in diseases that are not very well investigated. That means that the datasets generated from these studies are precious and they are rare, there are few of them. So, using those datasets and applying technology to generate insights from that data can help us provide health solutions to the communities who need it the most.
This interview was recorded in January 2024